Note: Due to a NDA with UPMC, I cannot reveal our findings or end solution. Here, I will focus mostly on our process.
Improve patient engagement
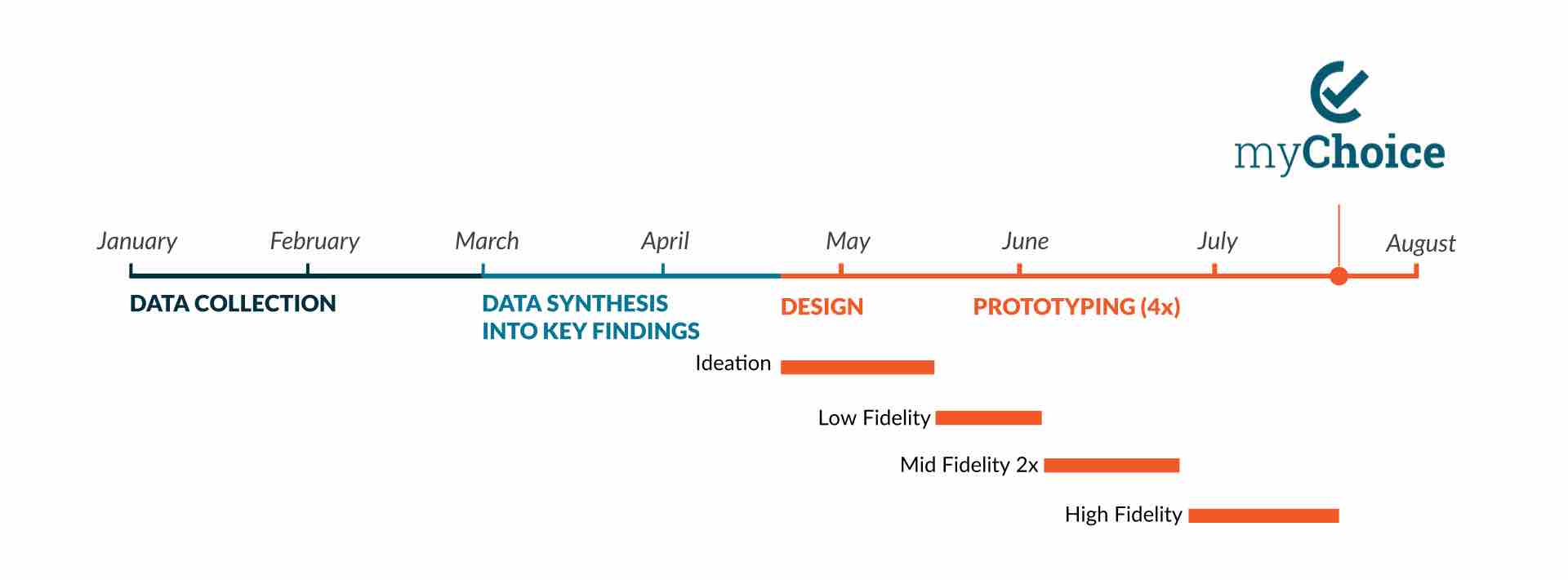
As a culmination of Carnegie Mellon’s Master’s of HCI program, this 8-month project was sponsored by the University of Pittsburgh Medical Center (UPMC) to look into a patient-facing tool with the goals of deeper engagement with the health system and better health outcomes.
Over the course of the project, we conducted user research, ideated, refined and iterated our designs until we arrived at a high fidelity solution that was validated by our users.
Directed Storytelling
We recruited and interviewed over 20 patients to learn about their interactions with clinicians and the struggles they deal with day-to-day with regards to their diet.
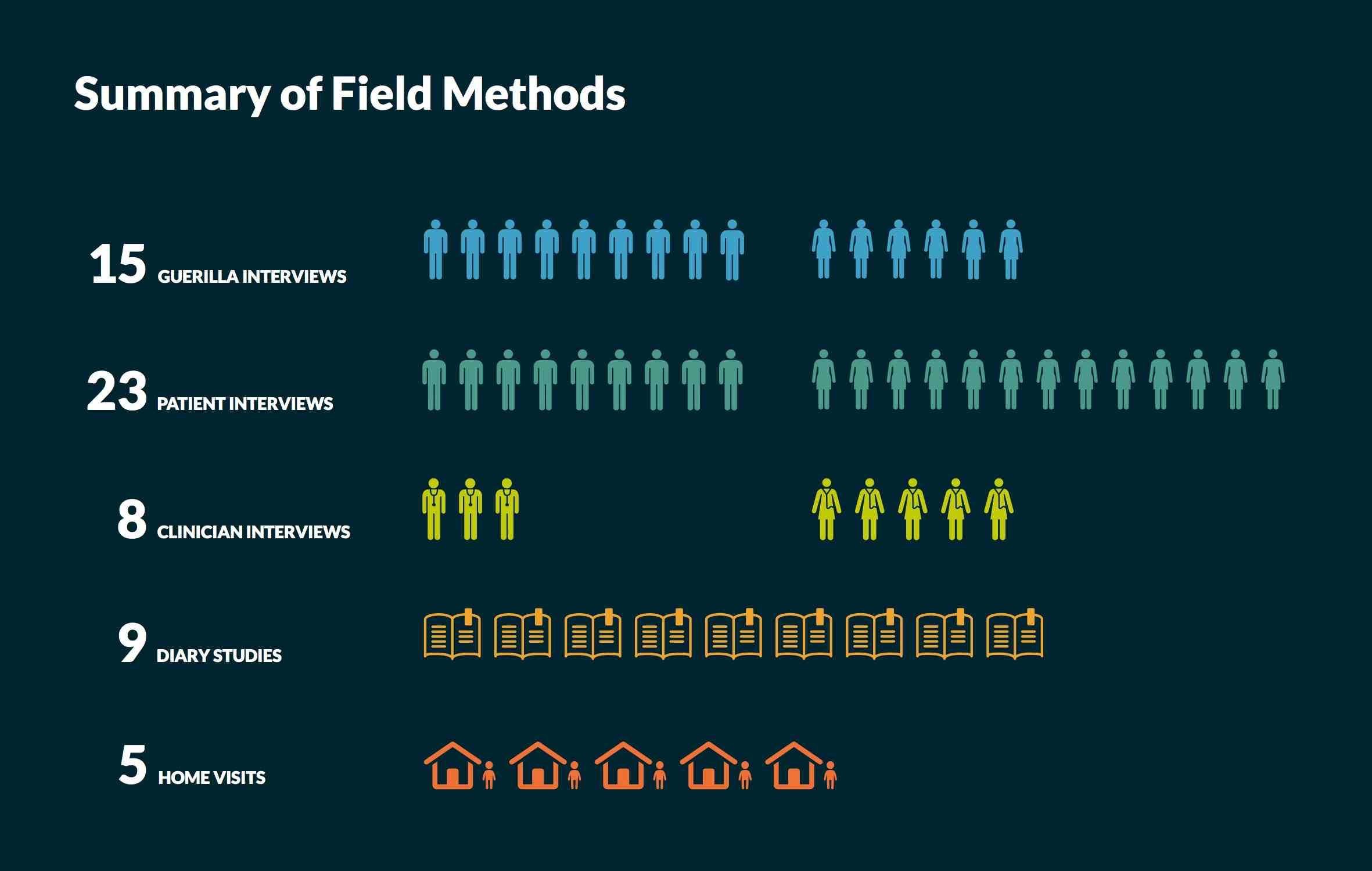
We also interviewed a range of clinicians, including nurses, cardiologists and a dietician to understand the challenges they encounter trying to improve the habits of their patients.
From these interviews, we extracted content to build affinity diagrams.
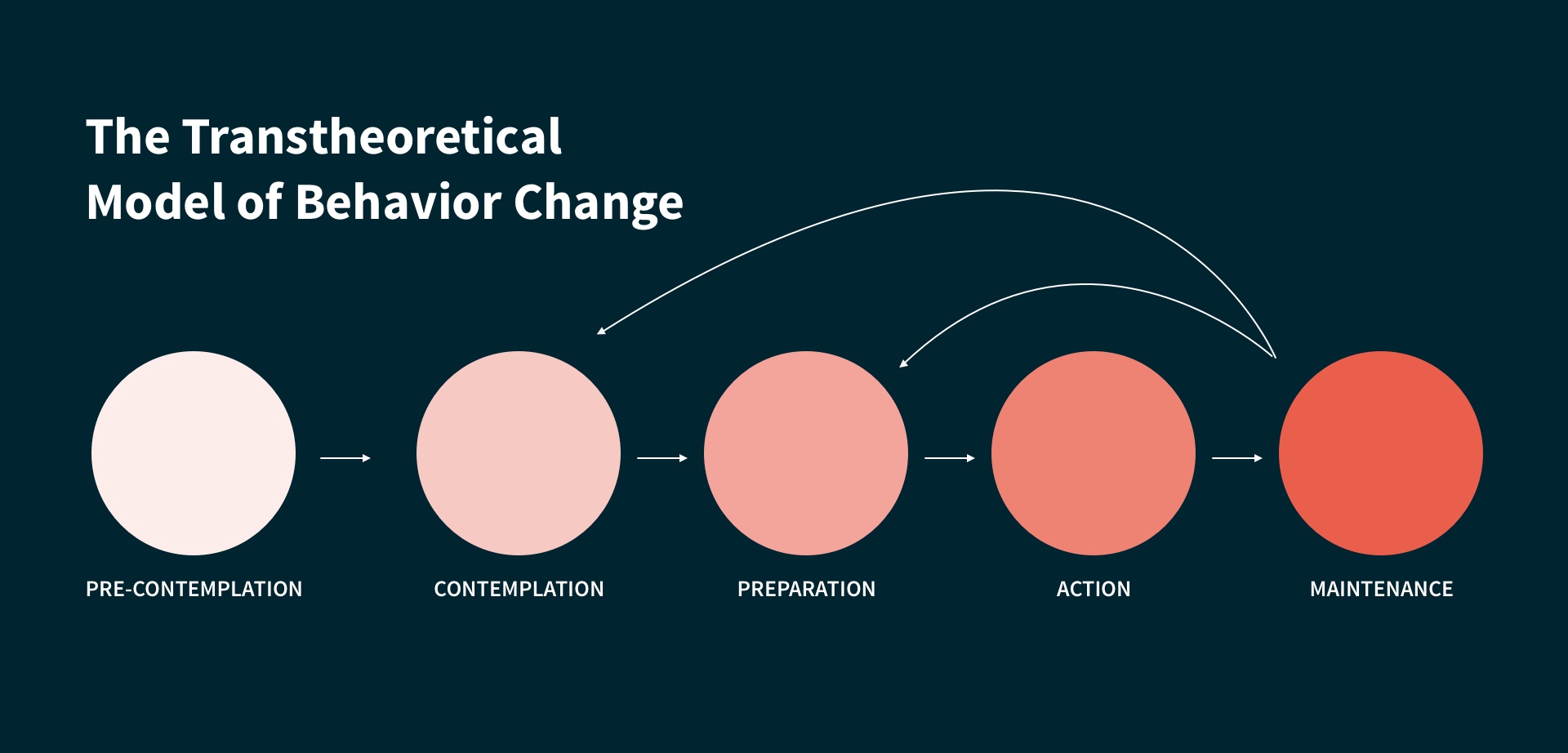
The Transtheoretical Model of Behavior Change
We researched literature relating to behavior change. Among them, we came across the Transtheoretical Model of Behavior Change which we felt was central to our goals of understanding the barriers people have to overcome along the journey of changing their behaviors.
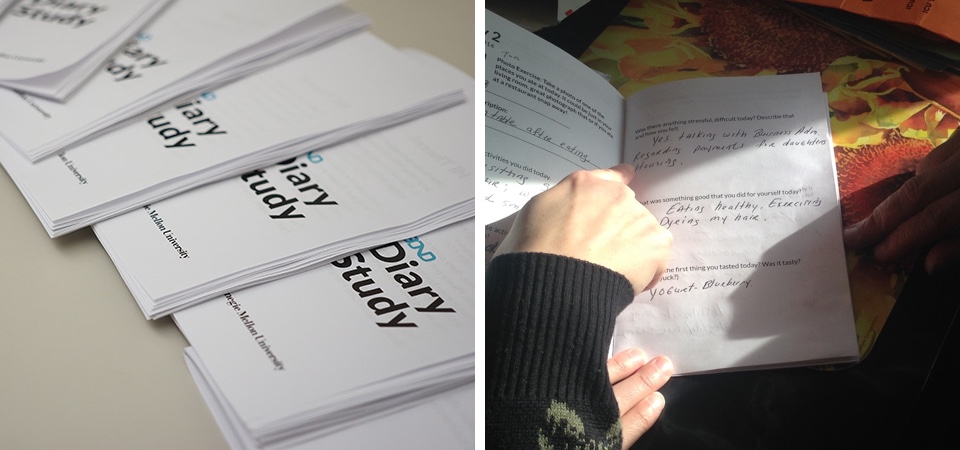
Diary Studies and Home Visits
We gathered nine participants for a weeklong diary study. Each day they answered questions about their day, for instance, what they did that made them feel happy and what stressed them. They also drew a picture to illustrate how their day went and took pictures of what they ate.
We visited the homes of some of these participants to learn about the environment they lived in and what a regular day for them was about.
Data Synthesis
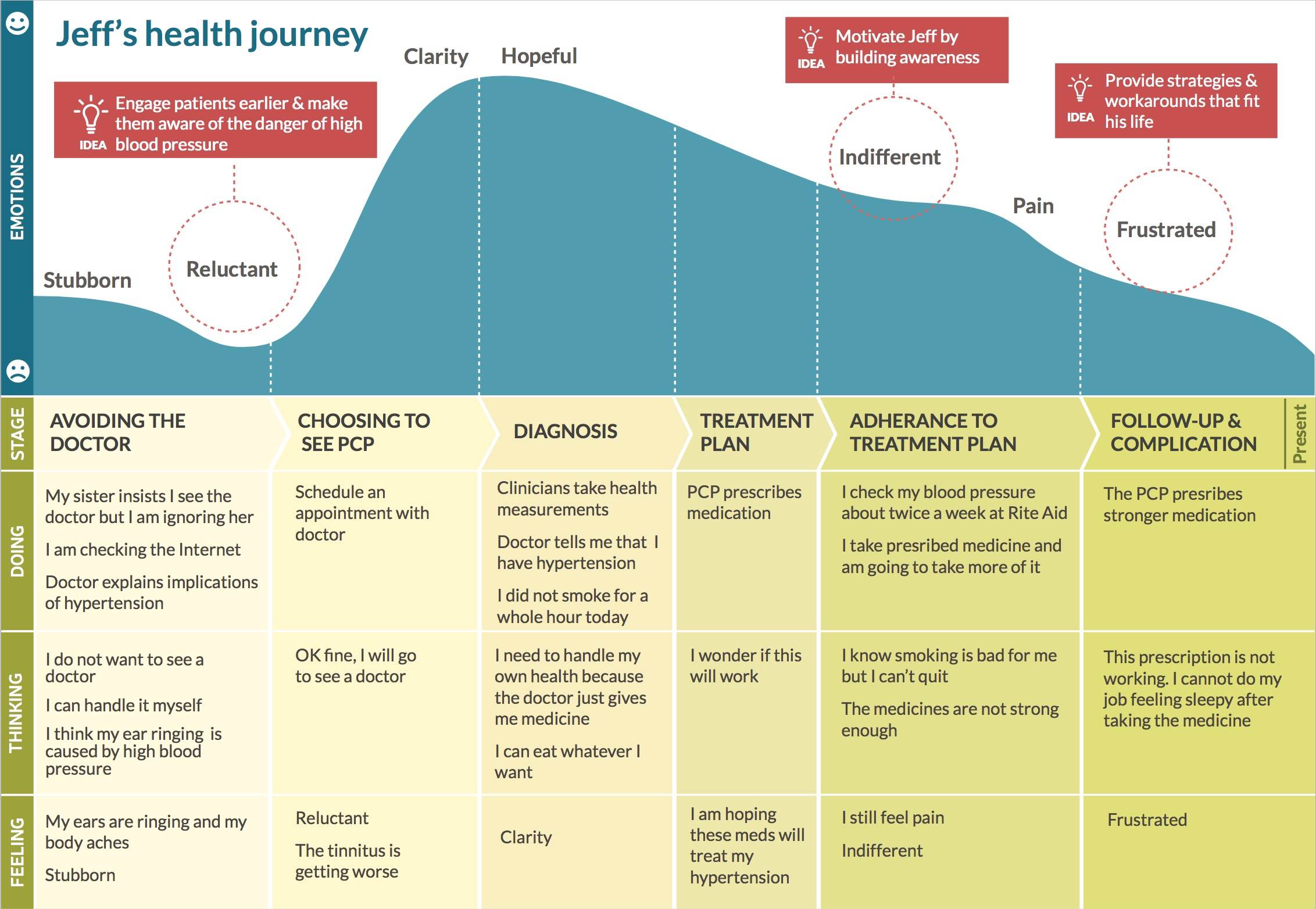
With a large amount of qualitative information, we synthesized them using affinity diagrams other different modeling techniques. After completing the field discovery, we also created a hybrid flow and cultural model, personas, and customer journey models.
From our key findings, we created personas and journey models to help the team and UPMC to better empthatize and relate to the patients.
Refining 50+ visions to one idea
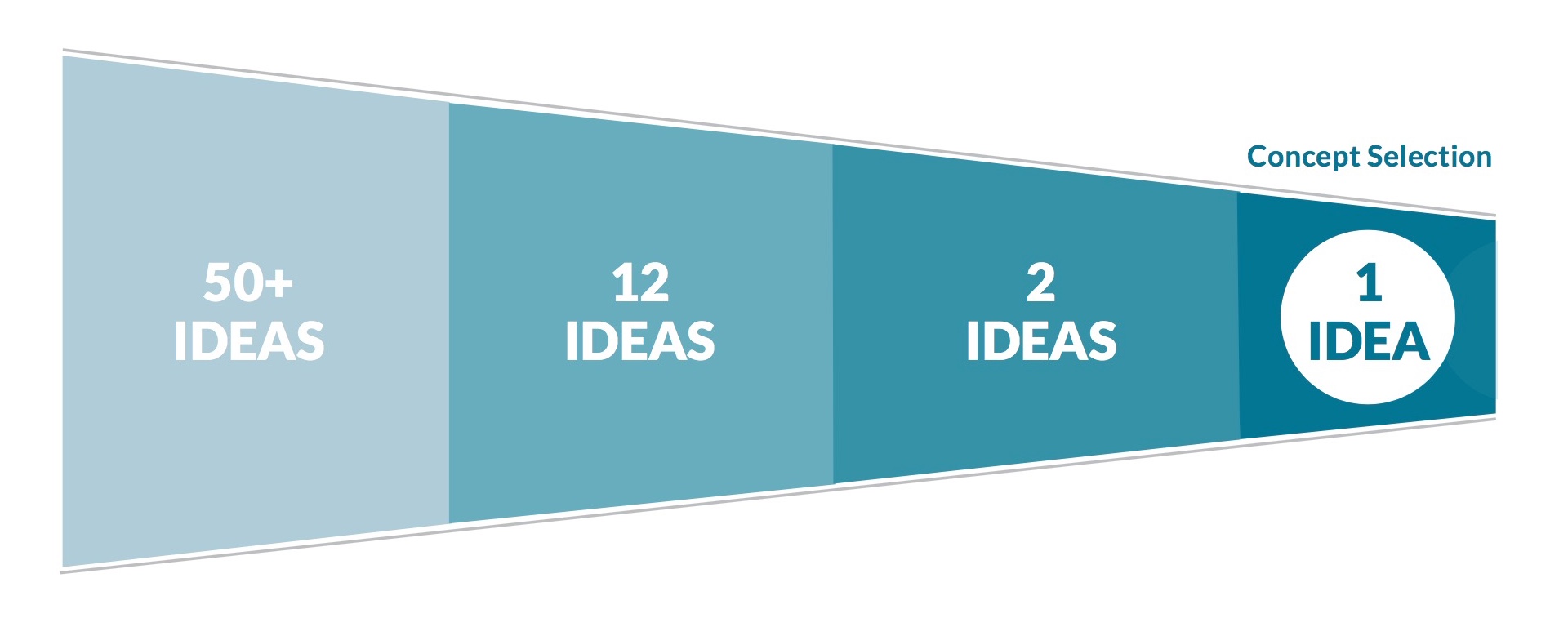
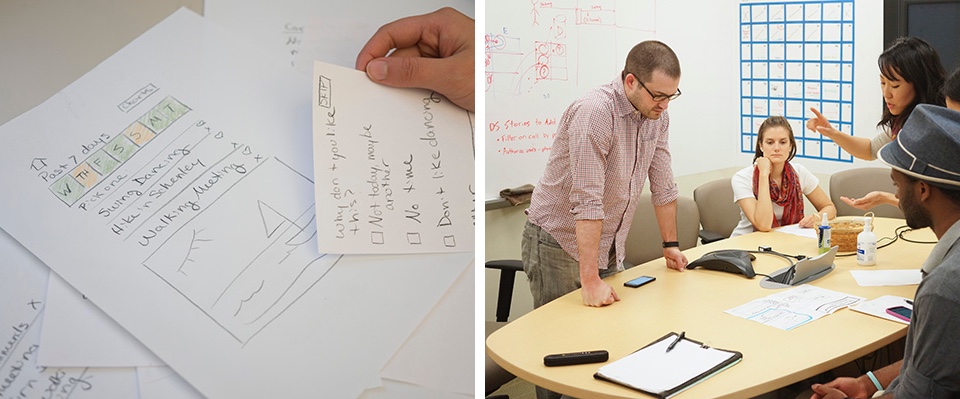
Informed by our prior research, we generated over 50 design visions for the final product. We then refined them to 12 distinct ideas that we then developed storyboards for, in order to speed date with patients.
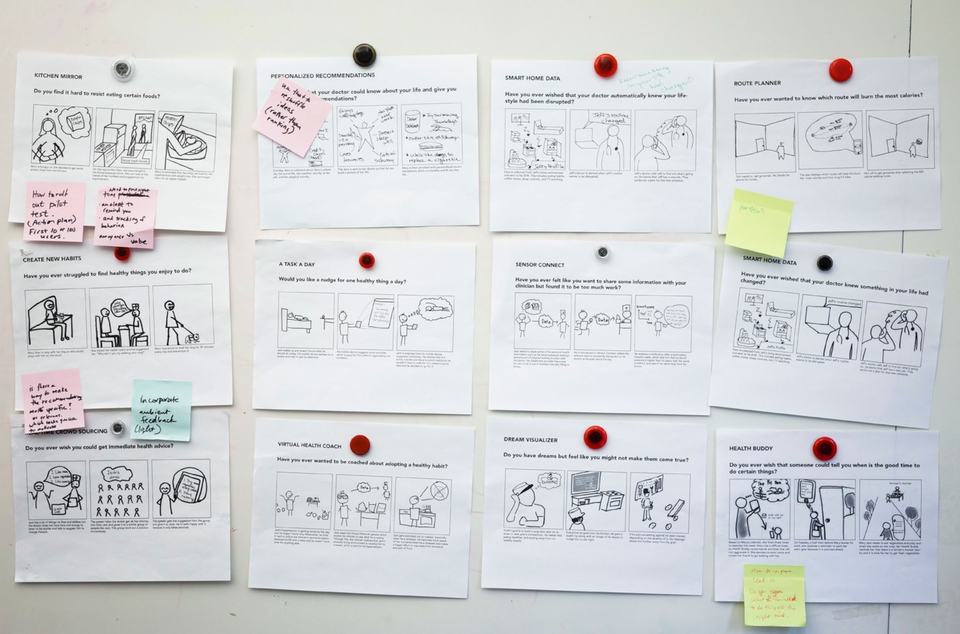
Based on feedback from the speed dating, we pulled the strongest features into two complete service design concepts for UPMC. After reviewing these concepts, UPMC selected the one with the strongest business value.
Prototyping: Getting from idea to validated solution
Over the course of the project we built four different types of prototypes to validate different aspects of our solution.
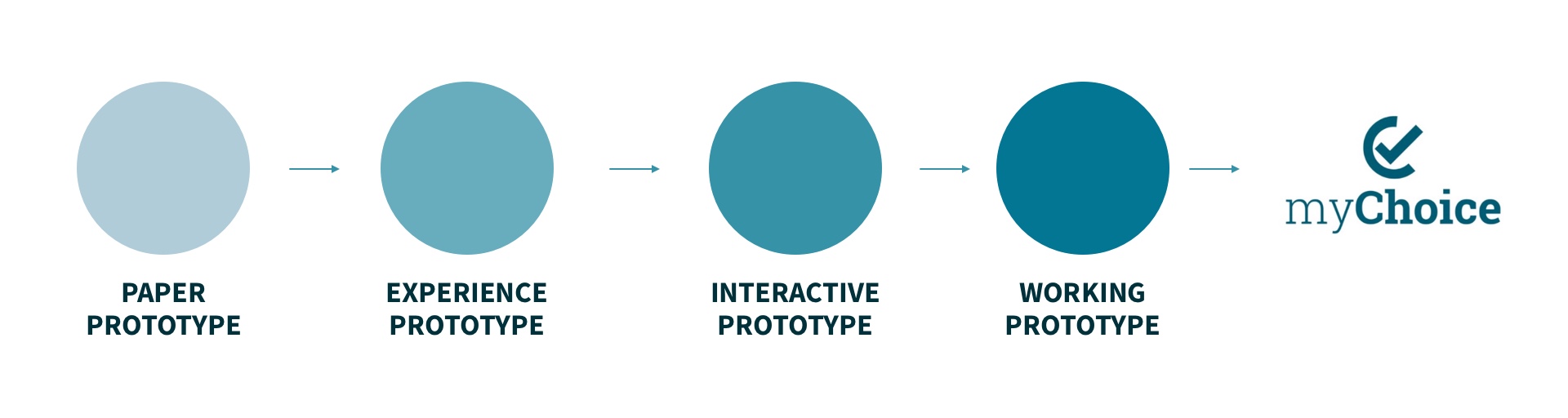
Paper prototypes to validate the general idea and to iterate on the fly during testing with participants.
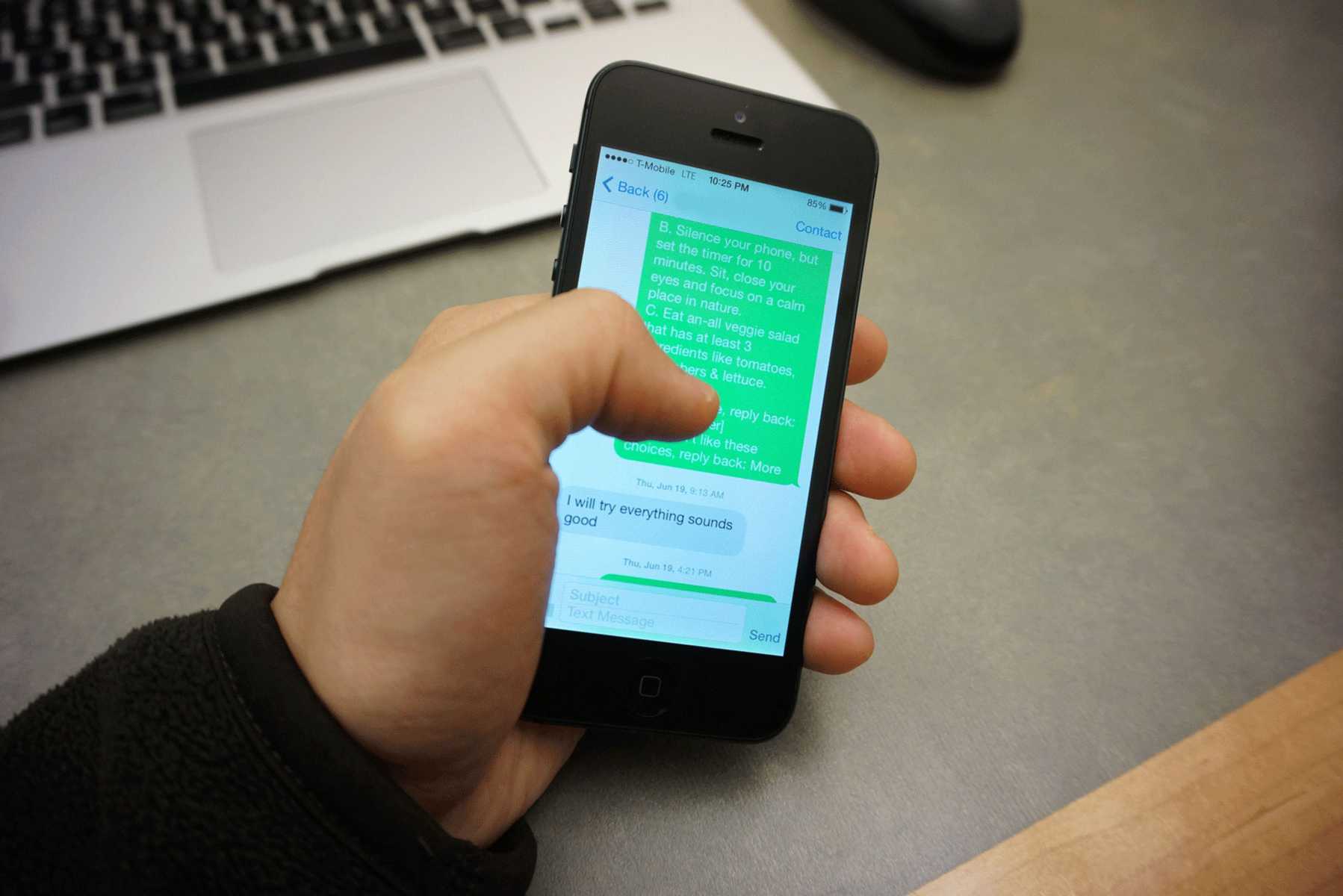
Experience prototypes to validate the service. We sent SMS messages to participants when they were at appropriate times and locations to mimic a context-aware intelligence.
Interactive prototypes to validate usability. We built a prototype using Balsamiq to learn about how patients might use the app, and the issues they would encounter as they were using it.

A working prototype to validate prolonged usage. We built a prototype using HTML, Cordova and PhoneGap and deployed it as an Android App so that our participants could use it in real-world settings. We tracked their locations in real-time and used the Parse service to send push notifications at appropriate moments.
A concept video to communicate how our solution could impact the lives of the patients we were designing for to various stakeholders, so they could envision how it would work from the perspective of the patients.
At the conlusion of the project, we delivered a solution to UPMC that was validated, along with all the research that led up to it so that they may further develop the product with greatly reduced risk.
About UPMC
The University of Pittsburgh Medical Center (UPMC) is an integrated global non-profit health enterprise that has more than 62,000 employees, 22 hospitals, and a 2.2 million-member health insurance division. They are also ranked one of top ten hospitals in the United States.